Paramedic Aid for Close Combat Injuries
This article on Emergency Paramedic Aid is for management of close combat injuries. Many times professional medical aid is far off and timely action by a paramedic trained soldier can help in saving life. The techniques described here are to be executed only by a trained paramedic soldier and not to be attempted by the untrained man as “First Aid”. Furthermore in most Indian urban and rural scenario, professional medical help is available nearby and the procedures described here may be unnecessary.
Contents Of A Paramedic Kit
1. Pain relief medication: Aspirin, ibuprofen and morphine. Gels for local application e.g. diclofenac gel.
2. Band-Aids, roller gauze for the dressing of wounds, splints, scizzors.
3. Equipment for emergency management of airway and breathing: Pocket mask for safe mouth to mouth respiration.
4. A stethoscope and blood pressure measuring apparatus.
5. Injection adrenaline, atropine, aminophylline, hydrocortisone and chlorpheniramine and tetanus toxoid.
6. Oral rehydration salts.
7. Wound closure kits.
8. Intravenous fluids like 0.9% saline, Ringers Lactate and Hetastarch 9. Snake bite kit.
Diagnosis Of Death
1. No carotid pulse
2. No heart sounds
3. No respirations
4. Deep coma
5. Dilated and unreactive pupils
6. Soldier not hypothermic or under influence of any drug or
intoxicant when above are tested.
Assessment Of A Severely Injured Soldier
A B C D E Format
A-AIRWAY: Is the airway open and unobstructed?
B-BREATHING: Is the soldier able to breathe?
C-CIRCULATION: Is there a palpable pulse in the neck? Are the hands warm and pink or cold and blue?
D-DISABILITY: Is the soldier conscious and able to communicate and walk? Does he have any fractures?
E-EXPOSURE: Is the body sufficiently exposed in order to evaluate all the injuries .
F-FOREIGN BODIES: Are bullets, knives or shrapnel embedded in the body.
G-GLUCOSE: Is he dehydrated and needing intravenous glucose? H-HYPO/HYPERTHERMIA: Is the soldier suffering from environmentally
induced severe changes in body temperature.
I-INFECTION: Is he running a fever suggestive of infection like wound infection, pneumonia, malaria (further the color of his lips, eyes or nails may suggest pathology)
OR
A – Airway & Cervical Spine Control
B – Breathing & Oxygenation
C – Circulation & Haemorrhage Control
D – Dysfunction & Disability of the CNS
E – Exposure & Environmental Control
PALLOR (paleness) of Nails, Face and Tongue may suggest anemia (low haemoglobin), low BP or Blood loss, CYANOSIS or Bluish coloration of the lips may suggest Hypoxia or low oxygenation, ICTERUS or yellow colora- tion of Nails and Sclera of eyes will suggest high Bilirubin, due to liver or blood related pathology.
Dysfunction & Disability Of The Nervous System
(Assessment of Mental Status) – An AVPU assessment is carried out:
A – Alert
V – Responding to Voice
P – Responding to Pain
U – Unresponsive
The soldier’s pupils in the eyes are examined for size, symmetry & reaction to torch light.
Concepts of Basic Life Support (BLS)
BLS is the support of circulation and respiration in a severely wounded soldier. The circulation is assessed by the pulse which can be palpated at the wrist and the neck. If the pulse is absent then it means that the heart is not pumping effectively and the chest has to be compressed to maintain the pumping action of the heart.
Respirations
Open the airway by head tilt and chin lift maneuver. Commence artificial respirations by forming an airtight seal with the mouth, closing the nose and watching the chest rise with each breath. 2 breaths after every 30 chest compressions. This should be done for a minimum of 20 minutes before abandoning efforts.
Basic Concepts Of Dealing With Severe Bleeding
1. Make the injured person lie down.
2. Remove any dirt or mud from the wound. Do not remove metal or other hard objects if they are very deep.
3. Apply direct pressure on the wound to stop bleeding.
4. Maintain this pressure for at least 20 minutes or until the bleeding stops.
5. Do not remove gauze or bandage used for pressure even if blood makes it wet. Add more material on the top of it.
6. Apply direct pressure on the artery if bleeding continues. E.g. in side of the arm just above the elbow or in the groin or behind the knee.
7. Do not move the injured part once bleeding has stopped.
Calculation Of Blood Loss And Management
The average human body contains 5 litres of blood. Using above table as a guide replace estimated amount of blood lost with equal volume of whole blood OR 4-5 times the amount lost with fluids like 0.9% sa- line. Insert large bore IV lines and give IV fluids as rapidly as possible. Infuse fluids to achieve a BP of 90/60 within 1-2 hours. Transfer rapidly to operative facility for definitive wound management.
Causes And Management Of Severe Pain
Causes: Fractures, severe sprains, bullet or knife injuries, blast injuries and burns.
Management: If fractures or sprains then immobilize the injured area, after which 2 types of medications can be given-aspirin and related com- pounds and morphine.
Aspirin can be given in a dose of 500 mg every 4-6 hourly. Ibuprofen can be given in a dose of 400 mg every 4-6 hourly. Both these medicines can cause severe stomach upset. Morphine can be given either by intravenous or intramuscular injection in a dose of 5-10 mg every 4 hourly or can be given orally in a dose of 60 mg every 4 hourly.
Snake Bite
1. Do not panic
2. Do not try to capture the snake
3. Immobilize the bitten part
4. Apply a loose splint if possible
5. Avoid a tourniquet
6. Avoid cutting the wound or sucking on it
7. Get to a medical centre to treat for poisoning
Viper Snake Bite
If no hospital available then a tourniquet can be tied proximal to the wound. It should not be so tight as to prevent blood flow through the arteries but should impede blood flow through the veins and the lymphatics. Suction devices are available to create a negative pressure over the bite so as to help remove the venom, however are not very effective. It is not recommended to make any incisions over the bite marks or to try and suck out the venom as the potential for causing harm is significant. The Sawyer Extractor comes with equipment needed for first aid treatment of a bite or sting, and for cleaning up of the bite site.
- Four plastic applicator cups (five possible suction areas to fit the bite, and bite location)
- Alcohol pads for wound clean-up andccleaning applicator cups between uses.
- Sting care pads.
- Topical anesthetic for pain relief.
- A book which gives instructions for treatment
This is a snake bite kit which uses the constrictor/suction method. It includes instructions, a tourniquet, antiseptic vials, a sterile lancet, a venom plunger pump which is adaptable to 3 sizes of suction area, and band aids to cover the wound when suction is complete.





Burns
1. Cool the burn by holding it under cold running water for at least 5 minutes.
2. Cover burned area with sterile gauze bandage.
3. Give a pain reliever like aspirin.
4. Don’t use ice or apply ointments to the burn and do not break burn – blisters.
5. Do not immerse very large severe burns in cold water as that could cause shock.
6. Chemical burns : Wash off any traces of the chemical and remove any clothing that has been contaminated, cover the burned area with sterile dressing
Fractures
Fractures are indicated by deformity, swelling, pain and inability to move the injured part, protruding bone, bleeding, or discolored skin at the injury site.
1. Stop any bleeding.
2. Immobilize the injured area and do not move the individual if neck or spine injury is suspected, wait for a trained doctor and keep the head, neck and back aligned when moving the person.
3. Apply splint if trained to do so i.e. immobilize the joints above and below the fracture.
Heat exhaustion or heat stroke
1. Move the individual out of the sun into a shady area.
2. Cool him by covering with damp sheets or spraying with
cool water. Direct air onto the person with sheets of paper or large leaves.
3. If conscious then make the person drink large amounts of water.
Choking
1. Give 5 blows on the persons back between the shoulder blades
2. Give 5 abdominal thrusts called as the Heimlich maneuver
3. Alternate blows and thrusts until the object is dislodged
Heimlich maneuver: Thrust the fist upwards into the abdomen using the other hand as support.
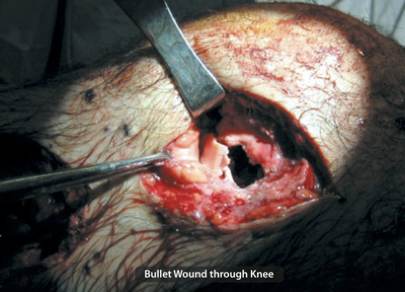
How to treat bullet or knife wounds
1. Do not immediately pull out any deep objects : Bullets, Knives or even arrows can sever arteries, removing them may cause
uncontrollable bleeding.
2. Control the bleeding : Direct pressure, limb elevation, pressure on main arteries and finally as a last resort a tourniquet – which may mean sacrificing a limb to save the individual.
3. Immobilize the injured area : Using splints and dressing as it will promote clotting.
4. Dress the wound to try and prevent infection.
5. Start giving rapid fluids by intravenous route if possible.
6. Transport to the nearest emergency medical facility.
Blast injuries
The effects of blasts fall into the following four categories:
a. Primary (Direct Effects Of Pressure)
(eg. overpressurization & underpressurization)
Rupture of tympanic membranes
Pulmonary damage
Rupture of hollow viscera
b. Secondary (Effects Of Projectiles)
Penetrating trauma
Fragmentation injuries
c. Tertiary (Effects Due To Wind)
Effects of structural collapse and of persons
Being thrown by the blast wind
Crush injuries and blunt trauma
Penetrating or blunt trauma
Fractures and traumatic amputations
Open or closed brain injuries
d. Quaternary
Burns, asphyxia, and exposure to toxic inhalants
Treatment
1. Attend immediately to any difficulty with breathing or a shock state by Basic Life Support as detailed above.
2. Control the bleeding.
3. Start intravenous infusions to combat blood loss.
4. Do not remove any deeply embedded fragments of metal or
shrapnel.
5. Arrange for immediate transport to an operative facility.
